The draft guidance, which is open to a month of public comment, is likely to stir a simmering medical debate over how widely genetic testing should be used to screen women for the BRCA mutations.
The Preventive Services Task Force, a volunteer panel of national experts, makes evidence-based recommendations for the primary care community.
Task force member Dr. Carol Mangione said most primary care providers take a patient's personal and family history of cancer into consideration when deciding whether to recommend a genetic test. Most, though, are unlikely to use the available standardized questionnaires to score a woman's risk for breast, ovarian, tubal and peritoneal cancers, said Mangione, a primary care physician and a professor of medicine and public health at the University of California, Los Angeles.
Geneticist Mary-Claire King, who discovered the BRCA mutations and their link to breast cancer risk in 1990, said she'd like every woman to be offered complete sequencing of BRCA1 and BRCA2 as part of routine medical care. She called the new recommendations "short-sighted" and "not based on the most recent data" and said they "could cost lives."
"What a shame," she told CNN in an email.
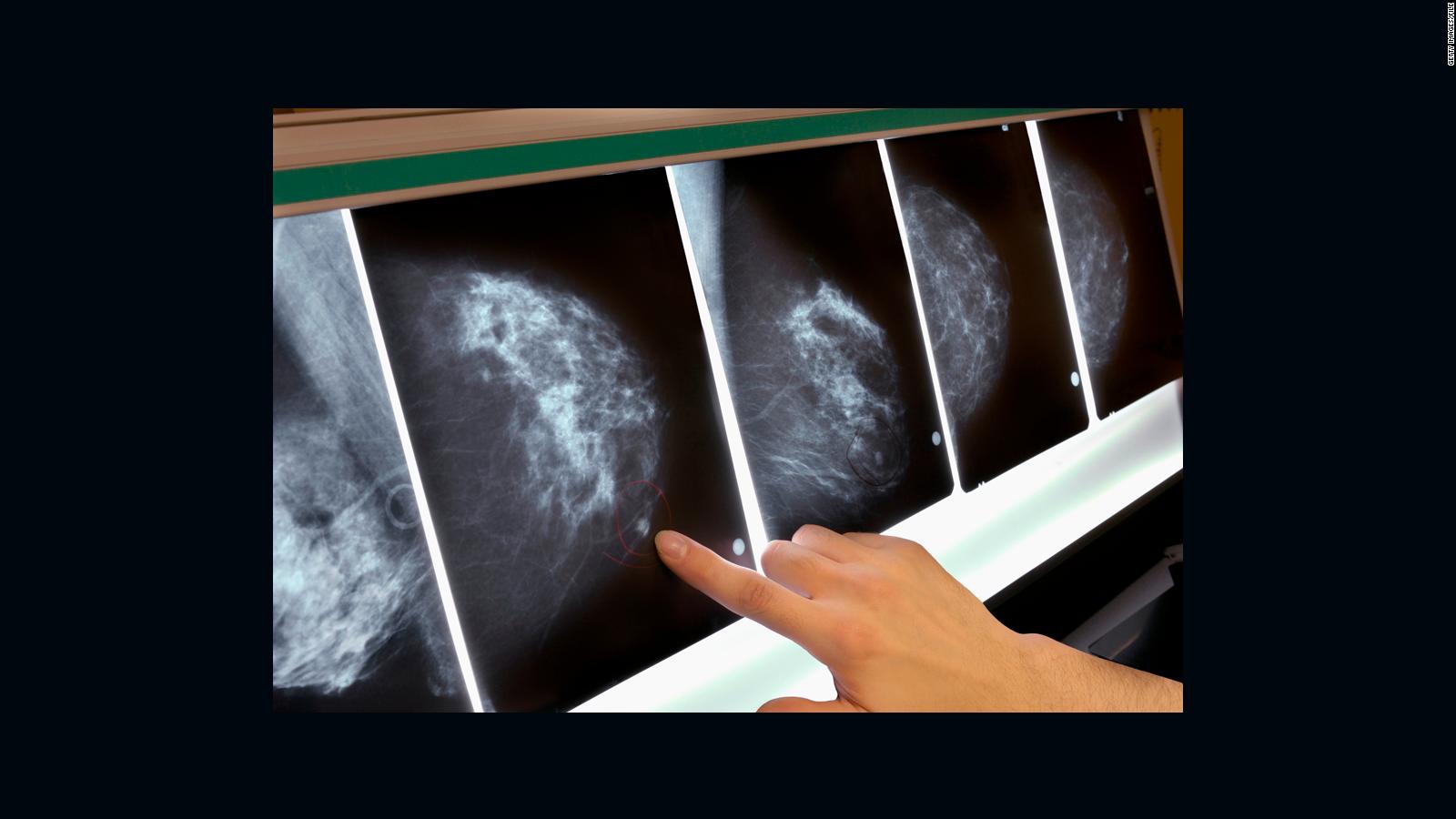
Using genetic testing to identify women who are at increased risk of breast cancer enables those women to take steps to reduce their risk, including undergoing enhanced or additional screening, chemoprevention and risk-reducing surgeries such as the type famously undergone by actress and UN Special Envoy Angelina Jolie.
Process begins with a patient questionnaire
Mangione said the new draft advocates a four-step process that begins with a standardized screening tool to determine whom to send on to genetic counseling. The standardized tests look at all known cancer risk factors, including whether the family history includes multiple cases of breast cancer rather than just one, as well as ethnic background, since some groups are more likely to carry BRCA mutations.
"The rates of these BRCA1 and 2 mutations in the general US population are around 0.2% to 0.3%, whereas in some special groups, such as women of Ashkenazi descent, the prevalence rates are closer to 2% -- so 10 times higher," Mangione said.
However, risk is a combination of many factors, she added, and the screening tool gives each woman a score that helps her primary care physician decide whether to refer her for genetic counseling.
After the second step of counseling, the third recommended step is a discussion between a woman and her health provider, and the fourth step is the testing itself.
Another "important part" of the new guidance is the task force's recommendation "against routine genetic counseling or testing in women who don't have a family history or ethnicity or ancestry associated with the increased risk of these mutations," Mangione said. "The potential harms of testing in low-risk women outweigh the potential benefit."
A genetic test may come back with "inconclusive results" or "uncertain significance," she noted. This could lead to anxiety, subsequent testing or even treatment that may be unnecessary, expensive or unsafe.
Some women get commercial genetic testing on their own. The new recommendation does not address these home kits, Mangione said, mostly because there hasn't been enough scientific analysis of this type of testing. "That can be fraught with a lot of problems if there isn't careful counseling beforehand to make sure that the benefits of the test outweigh potential harms."
Another view: Routine testing for all women
King, a professor of genome sciences and medical genetics at the University of Washington in Seattle who was not involved in formulating the task force recommendation, has very different advice for women and their providers.
"All women, regardless of personal or family history of cancer, should be offered complete sequencing of BRCA1 and BRCA2 as part of routine medical care at about age 30 or at their current age if they are already older," she said.
The only "meaningful" test is complete sequencing, said King, who said some, not all, home testing kits are "incomplete." That said, home testing kits that do offer complete sequencing may be good options for women who wish to learn whether they carry a mutation in BRCA1 or BRCA2, she said.
A complete medical genetic test need be done just once in a woman's lifetime, since her inherited DNA does not change, and "of course a woman could decline testing or decline at one time and change her mind later," she said.
Today, the technology is adequate and costs -- including the added cost for counseling -- are "very low" and "far less than most medical tests," she said.
"Primary physicians need not become genomics specialists themselves," King said. "For women who learn that they have damaging mutations in BRCA1 or BRCA2, primary physicians can do what they do best: appropriate medical followup of their patients."
King explained that "half of women with BRCA1 and BRCA2 mutations have no idea that they carry such mutations. So many women are in the dark because they inherit the mutation from an "unaffected father," so generally "there is no family history to trigger concern," she said.
The original guidelines for genetic testing of breast cancer patients were established about 20 years ago by the National Comprehensive Cancer Network, a nonprofit alliance of 28 cancer centers dedicated to improving patient care. At that time, genetic testing focused solely on BRCA1 and BRCA2 mutations and was both difficult and expensive.
Over two decades, additional "major" and "minor" gene mutations linked to breast cancer have become known. At the same time, genetic testing has become more advanced and far less expensive.
The Cancer Network's guidelines for who should be tested and who should not have evolved, but not everyone is satisfied. The American Society of Breast Surgeons, for example, published its own new guidelines last week recommending genetic testing for all patients diagnosed with breast cancer. The society based its new advice on the latest research, including one study that found the existing guidelines miss as many patients with hereditary cancers as they find.
Dr. Peter Beitsch, a cancer surgeon and co-founder of the TME Breast Care Network, a nonprofit focused on advancing treatment for breast cancer patients, said the reality is that genetic testing is "becoming ubiquitous, and recommendations like these are outdated" as soon as they are published because they are based on "research from the past, which is gathered even further in the past, and this field is moving rapidly."
The new recommendations are also confusing, said Beitsch, who was not involved in the process. Before screening a woman for increased risk of BRCA mutation, a physician must determine whether she is at increased risk of having one, he said, and this is a "Catch-22."
Still, he agrees with the task force that more research is needed across the field of genetic testing. "The tsunami of genetic testing is coming. Let's all prepare so we can deal with it in the best way possible."
Mangione emphasized that the new Task Force recommendation directs primary care doctors to "assess all women's family and personal history" and that it "is based on a review of all the available high-quality evidence around the benefits and harms of BRCA testing." She added that genetic counseling and testing for BRCA mutations "are recommended for some women because they are likely to be beneficial, but they are not for everyone" and concluded that women should talk with their doctors to find out "what assessments are right for them."
King believes that "sequencing for BRCA1 and BRCA2 will eventually be offered to all women. But it is a shame that women's lives will be lost in the meantime."
During the monthlong comment period, the general public as well as organizations and scientists can offer criticisms or support for the Task Force's new draft recommendation.






No comments:
Post a Comment